

|

Our Services / Cardiology Consultation / Cardiac Testings / Treatments
 Cardiology Consultation
Cardiology Consultation
We offer both office and hospital cardiology consultation for all types of cardiovascular problems. An office appointment with one of our cardiologists may be scheduled within 24 hours. The same-day appointment may be set up through your primary care physician's contact with our cardiologists.
Learn more from HeartAuthority about why and how we test your heart. »
Cardiac Testings
 Exercise Stress Testing:
Exercise Stress Testing:
An office schedule for an exercise stress test may be obtained through your primary care physician's office or through our cardiologists. The test may be scheduled within 24 hours and the same-day schedule may be set up through your primary care physician's contact with our cardiologists. The result of the test should be available to your primary care physician within 24 hours. Your primary care physician will be urgently informed of any significant abnormal findings.
Cardiac stress testing is usually performed to screen for blockages in the heart arteries or to estimate future outcomes of patients with known heart disease. There are two parts to the stress testing. First is the method of stress (walking or chemical stress testing). The second is the method of seeing the strain on the heart muscle (ECG alone or combined with heart imaging - sonogram or isotope imaging). The best method of the stress testing is the walking stress test if the patient is able do so. It is conventionally done on the treadmill, which starts slowly and speed and elevation are increased every three minutes until the patient has achieved adequate stress on the heart according to a calculated age-related heart rate. After the peak exercise, the patient cools down on the treadmill for a couple of minutes before stopping. The ECG is continuously monitored in all patients during stress. Many patients may also have heart image taken before and after stress testing for comparison. The capacity to exercise may also provide predictor of future heart event. With increasing age, obesity, and other ailments such as emphysema, or back, hip or knee problem, many patients may not be able to exercise adequately to stress the heart. In such patients, a chemical stress test may be a better choice. Some low level exercise may remain useful in some chemical stress test as the exercise may reduce the side effect of the drug used.
Stress testing is a very good but imperfect method of screening for heart artery blockages. While the stress test with an ECG monitoring alone may be adequate for some patients, the addition of heart imaging to the stress test may increase the accuracy of the test.
Learn more from HeartAuthority about coronary artery disease. »
Learn more from the American Heart Association about exercise stress testing. »
Learn even more from the American Heart Association about exercise stress testing. »
 Echocardiogram:
Echocardiogram:
An echocardiogram is an ultrasound test of the heart that takes about half an hour to one hour to perform and carries no significant risks. The test is used to evaluate how well your heart muscle is pumping. An echocardiogram with doppler study, which utilizes an ultrasound imaging in conjunction with blood flow study can assess heart valve motion and function accurately. The test can also detect if there is any abnormal fluid build-up around the heart. With the injection of saline (salt water), holes in the heart may become apparent. Contrast agents can also be used with an echocardiogram to see if there are large clots present in the heart chambers.
Learn more from HeartSite about echocardiogram. »
Learn more from the Mayo Clinic about echocardiogram. »
Learn more from WebMD about echocardiogram. »
 Transesophageal Echocardiography (TEE):
Transesophageal Echocardiography (TEE):
A TEE is an ultrasound test of your heart obtained through your food pipe as it goes behind and under your heart. You will be sedated and your throat will be made numb with a lubricating gel. You will be assisted to swallow an imaging instrument(a probe), which is similar to a scope used by a gastroenterologist to examine patient's food pipe and stomach lining. Most patients do not remember the test once it is over. A TEE is done when the usual echo images are not optimal for interpretation or there is a need to assess for clots in the back of the heart. It is also often performed in patients with suspected defective or artificial heart valves to look for clots or vegetations. If a hole in your heart is detected with salt water injection during a regular echocardiogram, the TEE will provide more accurate pictures of the hole to plan a treatment.
Learn more from HeartSite about Transesophageal Echocardiogram. »
 Heart Rhythm Monitoring:
Heart Rhythm Monitoring:
An office appointment for a 24-hour or 30-day heart monitor may be obtained through your primary care physician's office or through our cardiologists. The test may be scheduled within 24-48 hours and the same-day schedule may be set up through your primary care physician's contact with our cardiologists. The result of the test should be available to your primary care physician within 24-48 hours after the recorder is returned to our office. A longer heart monitoring may be necessary in some unusual situation and this may be done with an implantable device as small as a stick of chewing gum. The device is implanted similar to a pacemaker and it may be left in for up to 18 months. This procedure requires a minor incision and can be done as an outpatient. The device may be periodically evaluated with a computer program in the office using a tool similar to a pacemaker check, if needed.
Learn more from HeartAuthority about heart rhythm problems; see "What is an Arrhythmia?". »
 Peripheral Arterial Disease:
Peripheral Arterial Disease:
Blood vessels elsewhere in the body can become clogged up with cholesterol build-up just like arteries in the heart. This is called peripheral arterial disease.
The three simplest tests that are used to detect PAD are Carotid Doppler, Abdominal Aortic ultrasound and Ankle-Brachial Index (ABI). These tests are quick and carry no significant risks or discomfort.
Carotid Doppler is an ultrasound test of the neck artery supplying blood to your brain to look for any blockages. It uses the same machine that is used to image heart structures with ultrasound. A different imaging instrument, a probe, is employed for the neck arteries.
Abdominal Aortic Scan, which is an ultrasound test of the main blood vessel supplying your abdomen and legs is obtained with the same machine used for cardiac ultrasound test.
Ankle Brachial Index is a test that compares blood pressure readings in your arms and legs. Normally blood pressures in the legs are higher than the arms. If the leg arteries start clogging off (commonly in smokers), the blood pressure in that leg will fall below the arm pressure. The pressures are taken in the thigh, leg and toes and compared with the pressure in the arms.
Learn more from HeartAuthority about Peripheral Arterial Disease. »
 Cardiac Catheterization:
Cardiac Catheterization:
Cardiac catheterization is a procedure that is performed to evaluate the heart arteries, heart muscle and heart valves by taking real-time images of the arteries and main pumping chamber with X-ray equipment, specifically designed for this purpose. Measuring of pressures within various heart chambers may be needed to provide additional data to make the diagnosis. This procedure is typically performed in a cardiac catheterization laboratory within a hospital or at an out patient facility.
Learn more from HeartAuthority about heart attacks. »
 Physiologic Lesion Assessment:
Physiologic Lesion Assessment is a special technique that is used to assess the exact effect of the artery blockage on the blood flow to the heart muscle and this may be performed in continuation of the regular dye test. This assessment will determine the need for the treatment with balloon, stent, or bypass procedure to restore normal blood flow to the heart muscle. This technique is called fractional flow reserve (FFR), in which a special tiny metal wire, a guidewire, is used to measure the pressure generated before and after the narrow area in the heart artery. There will be a substantial drop of the pressure reading after the blockage if the blockage is of significant degree and the patient will benefit from balloon or stent treatment to remove the blockage.
Physiologic Lesion Assessment:
Physiologic Lesion Assessment is a special technique that is used to assess the exact effect of the artery blockage on the blood flow to the heart muscle and this may be performed in continuation of the regular dye test. This assessment will determine the need for the treatment with balloon, stent, or bypass procedure to restore normal blood flow to the heart muscle. This technique is called fractional flow reserve (FFR), in which a special tiny metal wire, a guidewire, is used to measure the pressure generated before and after the narrow area in the heart artery. There will be a substantial drop of the pressure reading after the blockage if the blockage is of significant degree and the patient will benefit from balloon or stent treatment to remove the blockage.
 Peripheral Vascular Angiography:
Peripheral Vascular Angiography:
Peripheral Vascular Angiography is a procedure that is used to identify the severity and location of the blockages in blood vessels outside the heart, peripheral arterial disease. The peripheral vascular angiography is performed by inserting a small plastic tube into the artery of a leg or an arm, and x-ray dye is used to take pictures of the artery. The severity of the blockage will help determining the benefit of removing the blockage by balloon or stent treatment.
Treatments
 Balloon Dilation Procedure:
Balloon Dilation Procedure:
 Percutaneous Coronary Intervention (PCI) includes a variety of procedures that are used to treat patients with diseased arteries of the heart, caused by a build-up of fats, cholesterol, and other substances in the blood. This is commonly referred to as plaque build-up that may reduce blood flow to the heart muscle.
Percutaneous Coronary Intervention (PCI) includes a variety of procedures that are used to treat patients with diseased arteries of the heart, caused by a build-up of fats, cholesterol, and other substances in the blood. This is commonly referred to as plaque build-up that may reduce blood flow to the heart muscle.
PCI, which is performed by threading a slender balloon-tipped tube (a catheter) from an artery in the groin to a narrow spot in an artery of the heart is referred to as Percutaneous Transluminal Coronary Angioplasty (PTCA, coronary artery balloon dilation or balloon angioplasty). The balloon is then inflated, compressing the plaque and dilating (widening) the narrowed heart artery so that blood can flow more easily.
 Stent Procedure:
The stent procedure often accompanies the balloon angioplasty procedure. A stent is a wire mesh tube that is used to prop open a heart artery during angioplasty. The stent is collapsed to a small diameter and put over a balloon catheter. It's then moved into the area of the blockage. When the balloon is inflated, the stent expands, locks in place and forms a scaffold. The stent stays in the artery permanently and it holds the artery open to improve blood flow to the heart muscle. Stents are used depending on certain features of the artery blockage, including the size of the artery and the location of blockages in the artery. Stents also help restore normal blood flow and keep an artery open if it has been torn or injured by the balloon catheter. Stenting is a fairly common procedure and it now represents 70-90 percent of PCI. Reclosure (restenosis) of the artery after the stent treatment is also a problem with the stent procedure. New types of stents, called drug-eluting stents, have been used in recent years. The stents are coated with drugs that are slowly released to prevent the blood vessel from reclosing.
Stent Procedure:
The stent procedure often accompanies the balloon angioplasty procedure. A stent is a wire mesh tube that is used to prop open a heart artery during angioplasty. The stent is collapsed to a small diameter and put over a balloon catheter. It's then moved into the area of the blockage. When the balloon is inflated, the stent expands, locks in place and forms a scaffold. The stent stays in the artery permanently and it holds the artery open to improve blood flow to the heart muscle. Stents are used depending on certain features of the artery blockage, including the size of the artery and the location of blockages in the artery. Stents also help restore normal blood flow and keep an artery open if it has been torn or injured by the balloon catheter. Stenting is a fairly common procedure and it now represents 70-90 percent of PCI. Reclosure (restenosis) of the artery after the stent treatment is also a problem with the stent procedure. New types of stents, called drug-eluting stents, have been used in recent years. The stents are coated with drugs that are slowly released to prevent the blood vessel from reclosing.
 Patients who have had a stent procedure must take one or more blood-thinning agents. Aspirin and clopidogrel are commonly used in combination in most patients. Aspirin is used indefinitely; clopidogrel is used for one to twelve months, depending on the type of stent used. It is important that you do not stop taking clopidogrel without consulting your doctor. Metal detectors do not affect the stent. Patients with a stent should not get a magnetic resonance imaging (MRI) scan for at least four weeks after the insertion date. Patients who have had a stent procedure must take one or more blood-thinning agents. Aspirin and clopidogrel are commonly used in combination in most patients. Aspirin is used indefinitely; clopidogrel is used for one to twelve months, depending on the type of stent used. It is important that you do not stop taking clopidogrel without consulting your doctor. Metal detectors do not affect the stent. Patients with a stent should not get a magnetic resonance imaging (MRI) scan for at least four weeks after the insertion date.
 Rotablator Procedure:
Rotablator Procedure:
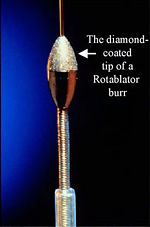 Sometimes plaque within the heart artery may contain a large amount of calcium that can make the blockage difficult to dilate or open. In this case a rotablator may be used to cut through the hardened plaque. A rotablator is a miniature drill capped with an abrasive, diamond-studded burr. The rotablator procedure is called Rotational Atherectomy, which is a minimally invasive treatment. During Rotational Atherectomy, the rotablator is guided to the blockage via a catheter through a blood vessel. Once the blockage is removed, an intracoronary stent insertion is usually performed to hold the clean artery open. The patient who receives a rotablator procedure will require similar post procedural care as in the stent only treatment. Sometimes plaque within the heart artery may contain a large amount of calcium that can make the blockage difficult to dilate or open. In this case a rotablator may be used to cut through the hardened plaque. A rotablator is a miniature drill capped with an abrasive, diamond-studded burr. The rotablator procedure is called Rotational Atherectomy, which is a minimally invasive treatment. During Rotational Atherectomy, the rotablator is guided to the blockage via a catheter through a blood vessel. Once the blockage is removed, an intracoronary stent insertion is usually performed to hold the clean artery open. The patient who receives a rotablator procedure will require similar post procedural care as in the stent only treatment.
 Patent Foramen Ovale (PFO) or Atrial Septal Defect (ASD) Closure:
Patent Foramen Ovale is a condition in which a natural communication between the two upper heart chambers remains open after birth. Whereas Atrial Septal Defect is the communication between the two chambers as a result of a birth defect. Too large a communication may allow blood flow from the left to right upper heart chamber and place a burden to the right heart circulation. Few patients may suffer recurrent strokes due to the cross-over of a blood clot from the lower part of the body into the left heart circulation. The potential excessive circulation burden and recurrent strokes are induications for PFO or ASD closure.
Patent Foramen Ovale (PFO) or Atrial Septal Defect (ASD) Closure:
Patent Foramen Ovale is a condition in which a natural communication between the two upper heart chambers remains open after birth. Whereas Atrial Septal Defect is the communication between the two chambers as a result of a birth defect. Too large a communication may allow blood flow from the left to right upper heart chamber and place a burden to the right heart circulation. Few patients may suffer recurrent strokes due to the cross-over of a blood clot from the lower part of the body into the left heart circulation. The potential excessive circulation burden and recurrent strokes are induications for PFO or ASD closure.
One or more tests will be done to measure the PFO or ASD and to make sure there are no other defects. An ultrasound imaging with an echocardiogram is used to estimate the size of the closure device needed. Another technique uses an ultrasound probe passed down the esophagus (transesophageal echocardiogram, or TEE) to allow your doctor to see the heart structures and blood flow in more detail.
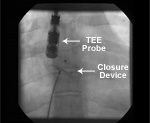 The cardiac catheterization procedure for a PFO or ASD closure typically takes 2 to 4 hours to complete. The catheter is initially inserted into a large vein in the groin area and then it is advanced into the heart. A local anesthetic is used to numb the area where the catheter was inserted. The use of general anesthesia or intravenous sedation depends on the doctor's preference and the patient’s need. A closure device is moved through the catheter to the location of the heart wall defect and the device is allowed to expand its shape to straddle each side of the hole. The device will remain in the heart permanently to stop the abnormal blood flow between the two upper heart chambers. The patient will not be able to feel the device. The cardiac catheterization procedure for a PFO or ASD closure typically takes 2 to 4 hours to complete. The catheter is initially inserted into a large vein in the groin area and then it is advanced into the heart. A local anesthetic is used to numb the area where the catheter was inserted. The use of general anesthesia or intravenous sedation depends on the doctor's preference and the patient’s need. A closure device is moved through the catheter to the location of the heart wall defect and the device is allowed to expand its shape to straddle each side of the hole. The device will remain in the heart permanently to stop the abnormal blood flow between the two upper heart chambers. The patient will not be able to feel the device.
Your doctor will prescribe medications that will need to be taken at home. Aspirin or other blood-thinning drug will need to be taken for 6 months or longer to prevent blood clots from forming. Do not stop taking the medication without talking with your doctor first. Antibiotics will also need to be taken 1 hour before certain medical procedures (for example, dental cleaning or certain surgeries) for up to one-year after device placement. It will be necessary to monitor the patient’s heart and device placement, at one month, six months, and one year.
The materials used in the closure device products have a proven long-term safety history and have been widely used in heart surgery procedures. It’s not likely that the body will have a negative reaction to these devices. Within a few days, the heart tissue will begin to grow over the device and it should completely cover the device by three to six months. The occluder device will not be affected by airport or other security sensors, household appliances, or medical imaging methods. However, the clarity of medical images may be slightly reduced because of the wire frame on the occluder devices. You will receive an identification card that should be carried with you to show to medical personnel if necessary.
Learn more from BCIS about Patent Foramen Ovale. »
 Renal Artery Stent Insertion:
Renal Artery Stenosis (RAS) is a medical condition in which one or both renal (kidney) arteries become narrow from cholesterol plaque build-up or overgrowth of blood vessel lining. RAS may lead to severe uncontrolled high blood pressure, kidney function impairment and symptoms of heart function impairment including severe chest pain and sudden fluid congestion with marked shortness of breath. Without an appropriate treatment, RAS may eventually become completely occluded and lead to renal function impairment. Currently RAS may be treated with a surgical or non-surgical procedure using balloon angioplasty or renal stent insertion. While balloon angioplasty for RAS has a less favorable outcome, renal artery stent treatment has been used for over a decade to optimize the non-surgical treatment.
Renal Artery Stent Insertion:
Renal Artery Stenosis (RAS) is a medical condition in which one or both renal (kidney) arteries become narrow from cholesterol plaque build-up or overgrowth of blood vessel lining. RAS may lead to severe uncontrolled high blood pressure, kidney function impairment and symptoms of heart function impairment including severe chest pain and sudden fluid congestion with marked shortness of breath. Without an appropriate treatment, RAS may eventually become completely occluded and lead to renal function impairment. Currently RAS may be treated with a surgical or non-surgical procedure using balloon angioplasty or renal stent insertion. While balloon angioplasty for RAS has a less favorable outcome, renal artery stent treatment has been used for over a decade to optimize the non-surgical treatment.
The screening procedure for RAS may be performed using an ultrasound of the kidney and its arteries or CT angiogram or magnetic resonance angiogram of the kidney arteries. Renal angioplasty is performed under local anesthetic and intravenous sedation primarily via leg artery access at the groin area. Patients remain in the hospital for 24 hours to monitor renal function and blood pressure response after the treatment.
 Peripheral Arterial Disease (PAD):
Peripheral arterial disease is a collective disease of the arteries that supply legs, arms, brain and other organs. Atherosclerosis or hardening of the arteries leads to a significant narrowing of these arteries and reduction in blood flow to these organs. With appropriate medical care and management of risk factors, patients can significantly reduce their health risks of developing PAD. Patients with PAD are also at high risk for heart attack and stroke. While PAD is common and affects over 10 million people, only one in four is diagnosed and receives treatment.
Peripheral Arterial Disease (PAD):
Peripheral arterial disease is a collective disease of the arteries that supply legs, arms, brain and other organs. Atherosclerosis or hardening of the arteries leads to a significant narrowing of these arteries and reduction in blood flow to these organs. With appropriate medical care and management of risk factors, patients can significantly reduce their health risks of developing PAD. Patients with PAD are also at high risk for heart attack and stroke. While PAD is common and affects over 10 million people, only one in four is diagnosed and receives treatment.
The treatment of PAD depends on the severity of symptoms, the degree and extent of arterial narrowing and patient’s overall health. Patients with PAD should be prescribed for therapeutic life style changes and medication to control their risk factors. Patients with open wound or chronic ulcer may require specialized wound care. Endovascular therapy or surgery may be necessary to reopen the arteries and improve blood flow.
Endovascular therapy is a non-surgical treatment for PAD that utilizes balloon angioplasty or stent insertion. The balloon angioplasty is performed by threading a slender balloon-tipped tube (a catheter) from an artery in the groin or elbow to a narrow spot in a limb artery. The balloon is then inflated, compressing the plaque and dilating (widening) the narrowed artery so that blood can flow more easily.
The stent procedure often accompanies the balloon angioplasty procedure. A stent is a wire mesh tube that is used to prop open an artery during angioplasty. The stent is collapsed to a small diameter and put over a balloon catheter. It is then moved into the area of the blockage. When the balloon is inflated, the stent expands, locks in place and forms a scaffold. The stent stays in the artery permanently and it holds the artery open to improve blood flow. Stents are used depending on certain features of the artery blockage, including the size of the artery and the location of blockage in the artery. Stents also help restore normal blood flow and keep an artery open if it has been torn or injured by the balloon catheter. Stenting is a fairly common procedure and it now represents 70-90 percent of the treatments.
Some plaque may contain a large amount of calcium deposit that may render the blockage hardened and resistent to balloon dilation. A rotablator is a miniature drill capped with an abrasive, diamond-studded burr, which is frequently used to pulverize the hardened plaque. The rotablator is used in a type of catheter-based procedure called rotational atherectomy. During rotational atherectomy, the rotablator is guided to the blockage via a catheter through a blood vessel. Once the blockage is removed, stent insertion is usually performed in conjunction with rotablator procedure.
Patients who have had a stent procedure must take one or more blood-thinning agents. Aspirin and clopidogrel are commonly used in combination in most patients. It is important that you do not stop taking clopidogrel without consulting your doctor. Metal detectors do not affect the stent. Patients with stent procedure should not get a magnetic resonance imaging (MRI) scan for at least four weeks.
Learn more from HeartAuthority about Peripheral Arterial Disease. »
 Permanent Pacemaker:
Insertion of a permanent pacemaker is a treatment that an outside electrical supply is being delivered to the patient’s heart to supplement the natural electrical activity of the heart muscle. The invention of a pacemaker is initially intended for the treatment of a slow heart beat either due to a worn out battery or a broken imaginary wiring inside the heart muscle, medically called heart block. As the technology of pacemaker has substantially evolved, the indication for pacemaker usage has also been expanded to include both specific type of rapid heartbeat and weak heart muscle associated with certain electrical conduction abnormalities.
Permanent Pacemaker:
Insertion of a permanent pacemaker is a treatment that an outside electrical supply is being delivered to the patient’s heart to supplement the natural electrical activity of the heart muscle. The invention of a pacemaker is initially intended for the treatment of a slow heart beat either due to a worn out battery or a broken imaginary wiring inside the heart muscle, medically called heart block. As the technology of pacemaker has substantially evolved, the indication for pacemaker usage has also been expanded to include both specific type of rapid heartbeat and weak heart muscle associated with certain electrical conduction abnormalities.
 Pacemaker insertion is an in-hospital procedure that requires a light general anesthesia and a one-day hospital. The procedure requires an insertion of one to three electrical wires and a battery. The preferred location of a pacemaker is over the left or right upper chest area, below the collarbone. In some special situations the battery may be inserted in the abdominal wall. The wire or wires are inserted in the vein and are threaded into the right heart chambers and positioned them according to the hearts need. In the one-wire system (single chamber pacemaker), the wire is positioned in the lower right heart chamber. The wires are positioned in the right upper and lower heart chambers in the two-wire system (dual chamber pacemaker). This is normally recommended in a patient who has a slow heart beat with normal electrical activity in the upper heart chambers. A third additional wire is positioned into a vein that drains into the lower right heart chamber and placed behind the lower left heart chamber in the three-wire system (biventricular pacemaker). This type of pacemaker is indicated in a patient with a weak heart muscle and an electrical activity abnormality. Pacemaker insertion is an in-hospital procedure that requires a light general anesthesia and a one-day hospital. The procedure requires an insertion of one to three electrical wires and a battery. The preferred location of a pacemaker is over the left or right upper chest area, below the collarbone. In some special situations the battery may be inserted in the abdominal wall. The wire or wires are inserted in the vein and are threaded into the right heart chambers and positioned them according to the hearts need. In the one-wire system (single chamber pacemaker), the wire is positioned in the lower right heart chamber. The wires are positioned in the right upper and lower heart chambers in the two-wire system (dual chamber pacemaker). This is normally recommended in a patient who has a slow heart beat with normal electrical activity in the upper heart chambers. A third additional wire is positioned into a vein that drains into the lower right heart chamber and placed behind the lower left heart chamber in the three-wire system (biventricular pacemaker). This type of pacemaker is indicated in a patient with a weak heart muscle and an electrical activity abnormality.
The pacemaker is normally checked with a computer scanner and a minor programming adjustment may be done before discharge the next morning. The patient will receive complete instructions regarding activity, incision care, pacemaker safety and follow-up appointment.
Learn more from HeartAuthority about pacemakers and defibrillators. »
 Implantable Cardiovertor Defibrillator (ICD):
An Implantable Cardiovertor Defibrillator is a device that is implanted into a patient to detect a serious life-threatening heart rhythm and deliver an electrical shock to correct it. ICD insertion is an in-hospital procedure that requires a light general anesthesia and a one-day hospital stay. The procedure requires an insertion of one to three electrical wires and an ICD generator. The device is slightly larger than a regular pacemaker unit and is also categorized similar to the pacemaker as a single chamber (one wire system), dual chamber (two wire system) and biventricular AICD (three wire system).
Implantable Cardiovertor Defibrillator (ICD):
An Implantable Cardiovertor Defibrillator is a device that is implanted into a patient to detect a serious life-threatening heart rhythm and deliver an electrical shock to correct it. ICD insertion is an in-hospital procedure that requires a light general anesthesia and a one-day hospital stay. The procedure requires an insertion of one to three electrical wires and an ICD generator. The device is slightly larger than a regular pacemaker unit and is also categorized similar to the pacemaker as a single chamber (one wire system), dual chamber (two wire system) and biventricular AICD (three wire system).
ICD implantation is initially recommended for a patient with a spontaneous or catheter induced life threatening heart rhythm. The indication of ICD implantation has recently been expanded for preventive treatment for patients who are at high risk of developing these serious life threatening heart rhythms. These include patients with markedly decrease in their heart function, less than 35% of the expected heart efficiency (approximately half of the normal heart function).
The ICD is normally checked with a computer scanner and a minor programming adjustment may be done before discharge the next morning. The patient will receive complete instructions regarding activity, incision care, ICD safety and follow-up appointment.
Learn more from HeartAuthority about pacemakers and defibrillators. »

|